Cabergoline
Transcript of Cabergoline

Colao, Lombardi & AnnunziatoCabergoline
Oncologic, Endocrine & Metabolic
Cabergoline
Annamaria Colao, Gaetano Lombardi & Lucio Annunziato
Department of Molecular and Clinical Endocrinology and Oncology,‘Federico II’ University of Naples, Italy
Cabergoline (CAB) (1-[(6-allelylergolin-8β-yl)carbonyl]-1-[3-(dimethyl-amino)propyl]-3-ethyl-urea) is an ergoline derivative with potent, selectiveand long-lasting inhibitory activity on prolactin (PRL) secretion acting ondopamine receptors present in pituitary lactotrophes. Receptor bindingstudies have demonstrated that CAB has high in vitro selectivity and affinityfor the subtype D2 of the dopamine receptor. In cultures of rat anteriorpituitary cells, the concentrations of CAB and bromocriptine required toinhibit PRL secretory activity by 50% (IC50) were 0.1 and 3.4 nmol/l, respec-tively. As compared to bromocriptine, CAB was more potent in inhibitingthe binding of [3H]N-n-propylnorapomorphine and it occupied the receptorfor longer. These effects were observed in all areas of the rat brain. In vivo,CAB at doses of 0.125 - 1 mg twice weekly caused a dose-dependentsuppression of PRL secretion in women with hyperprolactinaemia. CABwas shown to be significantly more effective than bromocriptine ininducing a complete biochemical response and clinical efficacy and wasbetter tolerated than bromocriptine in the majority of patients. Notabletumour shrinkage until tumour disappearance was observed during CABtreatment in most patients with macroprolactinoma. CAB was also shown tobe effective in patients resistant or poorly responsive to bromocriptine. Inview of the limited data on CAB-associated pregnancies and the longhalf-life of the drug, it is currently recommended that women seeking tobecame pregnant, once ovulatory cycles have been established, shoulddiscontinue CAB therapy 1 month before they intend to conceive.However, no data on negative effects on pregnancy or offspring have beenreported. The great efficacy of CAB together with its excellent tolerabilitymakes this drug the current treatment of choice for the majority of patientswith hyperprolactinaemic disorders. Very recently, the efficacy of CABtreatment has been reported in patients with acromegaly and clinicallynon-functioning adenomas with controversial results. CAB was alsoreported to have some efficacy in patients with Nelson’s syndrome andCushing’s disease although these data are available only for limited casereports.
Keywords:acromegaly, bromocriptine, cabergoline, dopamine agonists,growth hormone, hyperprolactinaemia, prolactin
Exp. Opin. Pharmacother. (2000)1(3):555-574
1. Introduction
Natural ergot alkaloids and synthetic ergoline derivatives display a remark-able variety of pharmacological activities depending mainly upon thenature and the configuration of substituents at position 8 [1]. The ergotalkaloids and derivatives have attracted great interest for their broad
5552000 © Ashley Publications Ltd. ISSN 1465-6566
Drug Evaluation
1. Introduction
2. Mechanisms of action
3. Pharmacologicalproperties of cabergoline
3.1 Pharmacodynamicproperties
3.2 Pharmacokineticproperties
4. Therapeutic applications
4.1 Hyperprolactinaemicsyndromes
4.2 Inhibition of lactation
4.3 Acromegaly
4.4 Clinically non-functioningadenomas
4.5 Cushing’s disease andNelson’s syndrome
6. Tolerability
7. Regulatory affairs
8. Conclusions
Acknowledgements
Bibliography
http://www.ashley-pub.com
Expert Opinion on Pharmacotherapy

spectrum of pharmacological action that includescentral, neurohumoral and peripheral effects. Such adiversity of biological activity does not allow theconsideration of these compounds as a singlepharmacological or therapeutical entity. There is noevidence suggesting that the diversity of biologicalproperties of ergot derivatives is due to a commonmechanism of action at the cellular or molecular level[2]. It is more likely that their wide range of biologicalactivities may be best explained by assuming thatergot compounds interact with more than onereceptor site, that the population of receptor sites theybind varies from organ to organ, and that affinity forreceptor sites and intrinsic activity vary fromcompound to compound [2]. The central, neurohu-moral and peripheral effects of ergot derivatives aremainly responses mediated by noradrenaline,serotonin, or dopamine receptors. No other group ofnatural products exhibits such a wide spectrum ofbiological action. Various ergot derivatives e.g.,bromocriptine, lisuride and pergolide, have shownpotent dopamine agonist (DA) properties and havebeen used as anti-Parkinson drugs and as PRL inhibi-tors [3]. CAB is an ergot derivative demonstrated topossess a potent and long-lasting PRL loweringactivity both in vitro and in vivo in different animalmodels [4]. CAB is the most recent DA included in thepharmacotherapy of hyperprolactinaemic syndromesworldwide. In the last decade several studies pointedout the efficacy of CAB in resolving the hyperprolac-tinaemic syndrome in the majority of patients,accompanied by a potent antitumoural effect onmacroprolactinomas and an excellent tolerance.Some other reports indicated that CAB could be alsoused in treating other types of pituitary adenomas,such as growth hormone GH-secreting, clinicallynon-functioning (NFA), and ACTH-secretingadenomas. This report aims at reviewing the currentknowledge on this drug in the endocrine field.
2. Mechanisms of action
Unlike other pituitary hormones, PRL secretion ispredominantly inhibited by dopamine secreted by thehypothalamus (Figure 1). Minor additional inhibitoryfactors act on γ-aminobutyric acid (GABA) andcholinergic pathways [5]. Oestrogens, thyrotropinreleasing hormone (TRH), serotonin, vasoactiveintestinal polypeptide (VIP) and endogenous opiatesact as stimulatory factors for PRL secretion, althoughtheir role is clearly minor compared to that of
dopamine [5]. The pituitary PRL secretory cellsexpress dopamine receptors, predominantly subtype2 (D2). DAs, such as CAB or bromocriptine, actdirectly at these receptors to inhibit PRL release [6]. Incultured rat anterior pituitary cells, the concentrationsof CAB and bromocriptine able to inhibit PRLsecretion by 50% of baseline (IC50) were 0.1 and 3.4nmol/l, respectively [7]. Similarly, receptor bindingstudies have demonstrated that CAB possesses higherin vitro selectivity and affinity for the D2 receptor thanbromocript ine, as the inhibi t ion ofN-n-propylnorapomorphine binding at the ratstriatum was 3 and 6 nmol, respectively [8]. Thecellular mechanism of PRL inhibition by DAs is far tobe fully elucidated. Although some cellular effectshave been demonstrated only with dopamine orbromocriptine, it seems likely that all dopaminergicergot derivatives, including CAB, share similarmechanisms of action. Stimulation of D2 receptors onpituitary lactotroph by dopaminergic agents reduceadenylate cyclase activity which, in turn, reducesintracellular cyclic AMP levels [9]. The inhibition ofcAMP levels is a key step in the hormone releaseinhibition by dopaminergic agents [10-12]. Otherintracellular mediators, such as calcium and phospha-tidylinositol, are known to be involved in PRLsecretion although their exact role has been stillpoorly elucidated. DAs reduce the size of prolac-tinomas, by inducing a reduction in cell volume (viaearly inhibition of secretory mechanisms, and lateinhibition of gene transcription and PRL synthesis [9]),as well as causing perivascular fibrosis and partial cellnecrosis [9,13]. Morphologic studies in rats treatedwith oestrogens, and CAB or bromocriptine, revealedthat CAB reduced the size of the cells and thegranules, and increased the number of granules perunit area of the cytoplasm [9]. These findings suggestthat CAB inhibits the maturation of PRL secretorygranules and the secretion of PRL more than itssynthesis. However, in the SMtTW tumour, a sponta-neous PRL-secreting transplantable tumour sensitiveto DAs, shrinkage under treatment and a regrowthafter bromocriptine and quinagolide withdrawal weredemonstrated for large tumours by in vivo ultrasono-graphic measurements of tumour size [14].Histological and ultrastructural effects were similar forthe two drugs: decrease in haemorrhage, reduction ofthe cell size and secretory activity, increase inimmunoreactive PRL cellular content, and inhibitionof exocytosis. There was no difference in the PRLmRNA content of treated and untreated tumours, asassessed by in situ hybridisation [14].
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
556 Cabergoline

3. Pharmacological properties ofcabergoline
3.1 Pharmacodynamic properties
CAB strongly inhibits PRL secretion both in vivo andin vitro. A significant inhibition of PRL secretion wasobserved within 12 h after treatment with CAB andbromocriptine in cultured pituitary cells fromoestradiol-induced rat pituitary tumours [15,16]. Theinhibitory effects of CAB and bromocriptine wereantagonised by sulpiride or haloperidol, and PRLinhibition was more pronounced with CAB thanbromocriptine treatment [16]. Inhibition of de novoPRL synthesis was better demonstrated in the CABgroup [16]. In various animal models, CAB markedlyreduced plasma PRL levels in vivo after single ormultiple doses, and the PRL-lowering effectsappeared 2 - 8 h after administration lasting for 72 h orlonger [17,18]. In addition, a single dose of CAB 0.6mg/kg to rats, significantly inhibited the serum levelsof PRL for 6 days [15]. Following a single dose of 0.6
mg/kg of bromocriptine, PRL levels were significantlyinhibited only at 6 h after administration [15].Continued oral administration of CAB significantlyreduced both PRL levels and the weight of thepituitary during 15 - 60 days of treatment as comparedwith BRC [15].
At single dose in healthy male volunteers, CAB 0.2 -0.6 mg produced a dose-dependent inhibition of PRLsecretion, 0.2 mg being the minimal effective dose.Maximal PRL suppression occurred within 5 h fromadministration at all doses [19]. At doses lower than 0.3mg, CAB exerted a significant PRL inhibition forapproximately 4 days while at doses of 0.4 - 0.6 mg forat least 7 days [19]. In 12 healthy men, single doses of0.5, 1.0 and 1.5 mg CAB produced a complete PRLsuppression (PRL < 1.0 µg/l) that occurred earlier andpersisted longer with the two higher doses [20]. Inhealthy women with regular menses, CAB doses of 0.4- 0.6 mg induced maximal inhibition of PRL secretionof 43 - 76% as compared to baseline [21]. After the low0.4 mg dose, PRL levels returned to baseline within 24
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
Colao, Lombardi & Annunziato 557
Stress
Prolactin
Suckling stimulus
Spinal afferent
Dopaminergic neurones
Peptidergic neurones
Serotoninergicneurones
DA
Drugs
AChNA
GABA
Srif
Histamin
- +
TRH
OpioidsVIP
Serotonin
Oestrogens
Figure 1: In contrast with the other pituitary hormones, prolactin secretion is mainly regulated by an inhibitory tone exerted bydopamine. Other neuromodulatory influences affect prolactin secretion either by inhibiting or stimulating its secretion.ACh: Acetylcholine; DA: Dopamine agonist; GABA:g-Aminobutyric acid; NA: Noradrenaline; Srif: Somatotropin release inhibitingfactor; TRH: Thyrotropin releasing hormone; VIP: Vasoactive intestinal polypeptide.

h, while the PRL inhibitory effects persisted until thefifth day after the administration of 0.6 mg [21].
Inhibition of progesterone secretion was observed inpregnant cats after administration of CAB sc. at thedose of 1.65 µg/kg/day for 5 days [18]. The decrease inprogesterone levels occurred after 3 - 4 days and waspreceded by a suppression of PRL levels [18]. A similarfall in progesterone levels was observed in pregnantbitches after administration of oral CAB at the dose of15 µg/kg/day [17].
Conversely, CAB did not modify the pre-ovulatory LHsurge nor the LH response to LHRH in rats [22]. Inhealthy humans or in patients with hyperprolac-tinaemia, CAB administration did not display anyeffect on GH, TSH or cortisol levels [19,23-25]. LHsecretion was reported to be unaffected by CABadministration by some authors [19,23-26], but a slightdecrease of LH and FSH after LHRH test was alsofound [27].
In addition, CAB, as with other DAs, seems to possessantimitotic effects [9]. In fact, it displayed antitumouraleffects on oestrogen-induced pituitary tumours[15,16,28,29] and 7-12-dimethylbenzanthracene-induced mammary tumours [29,30] in rats. CAB alsoreduced mean tumour weight of MXT-transplantedmammary carcinomas in mice [29].
3.2Pharmacokinetic properties
As therapeutic concentrations of CAB in the serum areat or below the detection limits of currently availableassay methods, pharmacokinetic studies of this drugare difficult [7, data on file, Pharmacia & Upjohn].However, by using radioimmunoassay with limits ofdetection of 12 ng/l in plasma, and 120 ng/l in theurine [31], and high performance liquid chromatog-raphy with limits of detection of 250 and 300 ng/l,respectively [32] have allowed calculation of the mainpharmacokinetic CAB parameters. The absolute oralbioavailability of CAB has not been established:studies using radiolabelled CAB showed that up to72% of the dose administered p.o. is eliminated in thefaeces within 10 days [33,34]. This suggests that CAB isabsorbed from the gastrointestinal tract but isextensively metabolised possibly with enterohepaticrecycling [34]. In contrast, less than 14% of theradioactivity excreted in the urine was due tounchanged drug [33,34]. The major metabolite is theacid derivative of CAB which, like the other metabo-lites, does not contribute to the pharmacologicalactivity of the drug [data on file, Pharmacia]. The
elimination of radiolabelled CAB was studied in asmall number of healthy volunteers [33,34]. After 24 h,< 10% of the total administered radioactivity wassecreted in the urine and none was present in thefaeces. After 240 h, the overall radioactivity excretedwas 10 - 20% in urine and 55 - 72% in faeces [33,34].
4. Therapeutic applications
A wide spectrum of therapeutic application iscurrently foreseen for CAB, besides the well knownuses in the field of hyperprolactinaemic syndromesand inhibition of lactation. In particular, some recentdata indicate that CAB can control GH and IGF-Ihypersecretion in acromegaly. CAB as adjuvanttreatment for NFA, has been tested in a small series ofpatients and two preliminary case reports have alsoindicated that CAB can be useful in ACTH hypersecre-tion. Some recent studies reporting the efficacy ofCAB treatment in pituitary adenomas are reviewed inthis section.
4.1 Hyperprolactinaemic syndromes
Hyperprolactinaemia is one of the most frequentclinical disorders in routine endocrine practice. Itcauses hypogonadism and/or galactorrhoea both inmen and women, as the most frequent presentingsymptom. Microprolactinomas (< 10 mm) ormacroprolactinomas (> 10 mm) are the most commoncauses of hyperprolactinaemia although thepathogenesis of the disorder is diverse (Table 1).Hyperprolactinaemia is noted in 15 - 20% of womenwith secondary amenorrhoea or oligomenorrhoea,approximately 30% of those with galactorrhoea orinfertility, and 75% of those with both amenorrhoeaand galactorrhoea [5,6,35]. In men, hyperprolac-tinaemia is often present for many years withoutsymptoms, as generally the most important symptomis the decrease in libido and/or sexual potency bothunderestimated by the majority of patients.Consequently, the mean age at diagnosis is 10 yearsgreater in men than in women [5,6,35]. This delay inthe diagnosis in men probably accounts for thegreater incidence of macroadenomas with visual fielddefects and hypopituitarism at first presentation, ascompared to women [35]. In particular, the presenta-tion of a prolactinoma in the elderly man was shownto be very heterogeneous and misleading: at the timeof diagnosis, hypopituitarism was more frequentamong older than younger patients despite a similartumour size [36].
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
558 Cabergoline

The aims of treating hyperprolactinaemia are tosuppress excessive hormone secretion and its clinicalconsequences (in particular infertility, sexual dysfunc-tion and osteoporosis), to remove tumour mass sorelieving disturbance in vision and cranial nervefunction, to preserve the residual pituitary function,and, if possible, to prevent disease recurrence orprogression. Before the availability of effective andwell-tolerated compounds to use in pharmaco-therapy, the approach to hyperprolactinaemia usuallyconsisted of surgical resection and/or pituitary irradia-tion. Generally, the management of prolactinomasinvolves considerations of medical therapy with DAs(overall the new compounds with selective activity onD2 receptors), radiotherapy or surgery, usually trans-sphenoidal, utilised alone or in combination (differentto when a micro- or a macroprolactinoma is involved)[39-41]. However, in recent years the medical therapywith DA has became the first therapeutic option in
prolactinomas [35,37-41]. This derives from theexperience accumulated for over 20 years with BRCthat was shown not only to inhibit PRL synthesis andsecretion but also to reduce cellular DNA synthesisand tumour growth: in more than 80% of patients,suppression of PRL levels and tumour shrinkage wasachieved with BRC given at doses of 2.5 - 5 mg/day[42]. Recently, two other D2 selective DAs, namelyquinagolide and CAB, became available for thetreatment of hyperprolactinaemia. Both drugs havethe advantage of being administered at doses lowerthan BRC thus inducing fewer side effects [43].Quinagolide was shown to be effective in mostpatients and was superior to bromocriptine in patientswith tolerance-related problems [43-48]. However, inseveral studies CAB was reported as excellent inresolving the hyperprolactinaemic syndrome[7,13,23-25,49,50]. In a multicentre study, 95% ofhyperprolactinaemic women showed a decrease in
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
Colao, Lombardi & Annunziato 559
Table 1: Causes of hyperprolactinaemia.
Type of cause Cause Example
Hypothalamic disorders Tumours
Infiltrative diseasesPseudotumour cerebriCranial irradiation
Craniopharyngioma, germinoma, third ventricle tumour, cyst,glioma, hamartoma, metastasisSarcoidosis, tuberculosis, Langerhans cell hystiocytosis
Pituitary disorders Micro- or macroprolactinomaAcromegalyCushing’s diseasePituitary stalk sectionEmpty sella syndromePseudoprolactinomas
Infiltrative diseases
Non-functioning adenoma, meningioma, intrasellar germinoma,metastasis that may produce functional stalk sectionGiant cell granuloma, sarcoidosis
Drugs Neuroleptics
Receptor blockersAntidepressantsAntihypertensivesOestrogensOpiatesPhenylalkylamine class N-typechannel calcium blockers
Perphenazine, fluphenazine, thorazine, promazine, trifluoperazine,haloperidol, chlorpromazine, dopamineMetoclopramide, sulpiride, domperidone, cimetidineAmoxapine, imipramine, amitriptylinea-Methyldopa, reserpine
Verapamil
Primary hypothyroidism
Chronic renal failure
Cirrhosis
Neurogenic Chest wall or spinal cord lesions,breast stimulation
Stress (physical orpsychological)
Idiopathic

serum PRL levels during chronic CAB treatment at thedose of 1 mg twice weekly [51]. In addition, CAB hasbeen shown to be more effective and better toleratedthan bromocriptine in a multicentre, randomised,24-week trial in 459 hyperprolactinaemic women [52].CAB treatment induced stable normoprolactinaemiain 83% of the patients compared with 59% of thosetreated with bromocriptine, ovulatory cycles orpregnancies were recorded in 72% of women treatedwith CAB and in 52% of those treated withbromocriptine [52]. Moreover, CAB induced signifi-cantly less frequent, less severe and shorter-lived sideeffects than BRC [52]. In a very recent retrospectivestudy including files from 455 patients [53], the
treatment with CAB normalised serum PRL levels in86% of them: in 92% of 244 patients with idiopathichyperprolactinaemia or microprolactinoma and in77% of 181 patients with macroprolactinoma. Sideeffects were noted in 13% of patients, but only 3.9%discontinued therapy because of side effects [53]. Themedian dose of CAB at the start of therapy was 1mg/week but could be reduced to 0.5 mg/week oncecontrol was achieved. In patients with macroprolac-tinoma a higher median CAB dose (1 mg/week) wasneeded as compared to those with idiopathichyperprolactinaemia or microprolactinoma (0.5mg/week) [53]. In patients with macroprolactinoma,CAB treatment at low weekly doses was also shown to
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
560 Cabergoline
0
25
50
75
100
PRL normalisation Tumour shrinkage
Pre
vale
nce
(%)
Naive
Intolerant
Resistant
Responsive
Figure 2: Prevalence of macroprolactinoma shrinkage after cabergoline treatment in our series. Shrinkage was evaluated as a > 80%tumour volume reduction as compared to basal values.
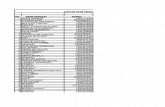
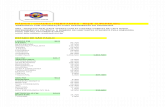
Table 2: Overview of efficacy of cabergoline treatment in patients with hyperprolactinemic disorders.
Author Year Ref. Totalpatients
Microadenomas Macroadenomas % PRLnormalisation
% Tumourreduction
% Sideeffects
Ciccarelliet al. 1989 [49] 30 27 3 81 71 48
Ferrariet al. 1989 [23] 46 38 8 85 83 15
Ferrariet al. 1992 [24] 127 108 19 90 79 23
Websteret al. 1993 [51] 162 161 1 92 40
Websteret al. 1994 [52] 223 223 0 83 68
Biller et al. 1996 [54] 15 0 15 73 73 ~ 0
Ciccarelliet al. 1997 [60] 48 26 9 91 70 4
Colaoet al. 1997 [73] 27 8 19 85 48 22
Colaoet al. 1997 [56] 23 0 23 83 61 4
Ferrariet al. 1997 [55] 65 0 65 61 66 25
Muratoriet al. 1997 [50] 26 26 0 96 68 24
Cannavòet al. 1999 [57] 37 26 11 92 100 8
Verhelstet al. 1999 [53] 455 249 181 86 67 13
Colaoet al. 2000 [58] 110 0 110 89 55 4.6

be successful in causing tumour shrinkage [54-57]. Inthese studies, it was demonstrated that 12 - 24 monthsof treatment with CAB induced marked tumourshrinkage with complete disappearance of tumourmass in 26.1 - 36.4% of cases. The majority of thestudies on macroprolactinomas included patientswho had never been treated with other DAs or whowere treated with BRC for brief period of time becauseof intolerance. In a multicentre study, CAB treatmentinduced tumour shrinkage in 60% of patientspreviously treated with other DAs and in 82.3% ofuntreated patients [55]. In another recent multicentrestudy [53] of 181 patients with macroprolactinoma,CAB treatment induced tumour shrinkage in 67% ofcases with improvement of visual field defects in 70%of patients. In a recent review of our cases whichincluded 110 patients with macroprolactinoma,notable tumour mass shrinkage was observed in themajority (88.5%) of patients [58]. Tumour massdisappeared in 57.7% of 26 naive patients. Tumourshrinkage and/or disappearance were also observedin patients previously treated with BRC orquinagolide, but to a lesser degree (Figure 2).Interestingly, in naive patients the tumour shrinkingeffect of CAB was very rapid, occurring even after thefirst administration of 0.5 mg of the drug (Figure 3).On the basis of these evidences, CAB has beensuggested as the first approach to patients withmacroprolactinomas [52-57]. Table 2 overviews theeffects of CAB in patients with hyperprolactinaemia.
Infertility and osteoporosis, are the two main clinicalconsequences of hyperprolactinaemia. The beneficialeffect of CAB treatment on the recovery of fertility inhyperprolactinaemic women has been widelyreported (see below), however, data on the recoveryof fertility in men are extremely limited. In a prelimi-nary study [59], we reported that CAB rapidly inducedthe normalisation of sperm quality, significantlyincreasing the sperm number already after the firstmonth of treatment at standard doses and earlier thanduring bromocriptine treatment in men with prolac-tinoma. The effects of seminal fluid characteristicswere similar after quinagolide and CAB treatment(Figure 4): this was due to the evidence that PRLlevels were normalised earlier during CAB andquinagolide treatments than during bromocriptinetreatment [41]. CAB recovered ovulatory cycles andinduced pregnancy in the majority of the studiesincluding women of fertile age [23-25,49-52,60]. DAshave not been associated with any adverse event onfoetal development or pregnancy outcome, but
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
Colao, Lombardi & Annunziato 561
A
B
C
Figure 3: Sagittal magnetic resonance imaging (MRI) of thesella turcica in one woman with macroprolactinoma before(A) and after 1 week (B) and 2 weeks (C) of cabergolinetreatment. The image B was collected just after 1 tablet ofcabergoline (0.5 mg). Thereafter the patient was treated with0.5 mg every 3 days. After the first week at the dose of 1 mg (3tablets) a second MRI control was performed. Enlargement ofthe third ventricle was evident after the first administration ofCAB while a clear-cut tumour decrease was observed after thesecond week of treatment.

experience with BRC is more extensive. Thus, forwomen requiring treatment for fertility, BRC remainsthe treatment of choice in most centres, whereas CABand quinagolide are acceptable second-line drugs inpatients intolerant or resistant to BRC [7,35,41,61,62].Recently, among 27 women treated with CAB whobecame pregnant, 25 delivered a healthy child: 1patient had an intended abortion and another amiscarriage [53]. Currently, there are no establishedguidelines to follow patients during pregnancy butlarge agreement exists to stop the drug(s) whenpregnancy occurs in patients with microprolactinomawhile it is preferable to continue the treatment in
those with macroprolactinoma so as to avoid the riskof tumour enlargement. Another possibility is to alsostop the treatment in patients with macroprolac-tinoma but apply a careful clinical follow-up in thesepatients. If the patient shows clinical signs ofexpanding lesion, such as headache or visual fielddefects, a sellar MRI can be performed and treatmentrestarted. In women with microprolactinoma notdesiring fertility, oestrogen replacement therapy canbe carried out, since it has been shown not to increasetumour size [63]. However, a second MRI should beperformed to exclude the occurrence of tumourenlargement in patients with oestrogen-sensitivetumours.
As far as osteoporosis is concerned, in women therecovery of hypogonadism, more than the suppres-sion of PRL levels, was associated with theimprovement of bone mass [64,65]. In men, the dataconcerning the recovery of bone loss are still scant[66-68]. The treatment with bromocriptine,quinagolide and CAB for 18 months induced a signifi-cant increase in bone mineral densi ty inhyperprolactinaemic males [69], but it did not signifi-cantly modify the T score (Figure 5) indicating that alonger period of treatment could be necessary to thisend. In addition, the age of onset of hyperprolac-tinaemia also played a relevant role in the potentialreversibility of osteopenia, as demonstrated by theevidence that in young/adolescent patients withprolact inoma, 2 years of treatment withbromocriptine, quinagolide and CAB, though normal-ising PRL levels in the large majority of patients, didnot significantly modify bone mass [70].
CAB was also shown to normalise serum PRL levelsand restore gonadal function in about 70% of patientsconsidered resistant or hypo-responsive to BRC[71-73]. The definition of therapy-resistance to DAs isstill a matter of controversy. However, true resistancecan only be documented by molecular biologystudies, demonstrating the absence or poor expres-sion of D2 receptors on the membrane surface oftumour cells [74,75] or abnormalit ies at apost-receptor level [76]. It is commonly accepted toclinically define the resistance to DA as the absence ofserum PRL level normalisation and/or tumourshrinkage after at least 3 months of treatment withbromocriptine (15 mg) or quinagolide (0.6 mg)[44,77,78]. These doses can be considered ratherelevated in the treatment of hyperprolactinaemia. Themajority of the patients, however, show partial, ratherthan complete, therapy resistance and an increase of
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
562 Cabergoline
0
10
20
30Basal 1 month 6 months
Spe
rmco
ncen
trat
ion
(10
/ml)
6
0
25
50
75
Mot
ility
(%)
0
25
50
75
Nor
mal
mor
phol
ogy
(%)
Bromocriptine Cabergoline Quinagolide
Figure 4: Sperm concentration (top), total motility (middle)and normal morphology (bottom) in hyperprolactinaemic mentreated with bromocriptine, cabergoline and quinagolide. Theincrease of sperm count was evident with all compounds butwas greater using cabergoline and quinagolide [41].

the drug dose is likely to induce normalisation of PRLlevels. The effectiveness of any treatment is strictlyrelated to tolerability and to patients’ compliance. Inthis respect, CAB induced a marked improvement inpatient compliance, thanks to the very low prevalenceof side effects and the possibility to take the drug onceor twice a week. In a previous study we demonstratedthat tolerability and compliance were better duringCAB than during quinagolide or bromocriptinetreatments [73]. In a recent re-evaluation of our cases,we observed normalisation of PRL levels in 19 of 37resistant patients (51.3%) after 6 - 12 months oftreatment with CAB at the dose of 1 - 2 mg/week andin the remaining 18 patients, normoprolactinaemiawas achieved after 18 - 24 months at 3 - 3.5 mg/week[58]. However, stable normoprolactinaemia wasachieved in 26 of the 37 patients [58]. At the end oftreatment, average tumour shrinkage was 58.4 ± 4.9%and significant tumour shrinkage was obtained in 10patients (29.4%) [58]. Sometimes the effects on tumourmass can be partially dissociated from those on PRLlevels, as recently described in a case report [79].However, not all patients responded satisfactorily toCAB and quinagolide, although the response to CABwas better in several cases [72,73].
In conclusion, CAB treatment was shown to beeffective in normalising PRL levels, so restoringgonadal function, and in shrinking tumour mass inmost patients with hyperprolactinaemia. Long-termtreatment with CAB was shown to be well-toleratedby the majority of patients and only mild side effectswere reported, compared to those reported withbromocriptine. In this light, CAB treatment can beconsidered the first choice in patients with
hyperprolactinaemia, even in children and adoles-cents [80,81], and in elderly patients [36]. However, thetreatment strategy could be reconsidered on the basisof the high cure rate of trans-sphenoidal adenomec-tomy [40,82], which might be further improved by useof new endoscopic techniques [83,84].
4.2 Inhibition of lactation
Absence of milk secretion was demonstrated inseveral trials using CAB [85-89]. CAB showed a cleardose-response relationship over the range 0. 4 - 1 mg:at these doses CAB was markedly more effective thanplacebo in preventing milk secretion and breasttension or tenderness [85,86,89]. Higher doses wereassociated with greater clinical efficacy and a morerapid reduction in PRL levels. In a large study investi-gating this issue [85], CAB at the dose of 0.5, 0.75 and 1mg induced a complete clinical response in 5, 70 and90% of women, respectively. By comparison withbromocriptine, CAB at the single dose of 1 mg waseffective in 90% of women, while bromocriptine, atthe dose of 2.5 mg twice daily for 14 days, waseffective in 84% [88]. As compared to bromocriptine,CAB was effective in inhibiting lactation earlier [88]. Inaddition, rebound breast symptoms in the thirdpostpartum week occurred in a significantly greaterpercentage of bromocriptine-treated women thanthose treated with CAB (24 vs. 5%) [88]. Conversely,there are no data concerning the efficacy of CAB insuppressing established lactation. In two unpublishednon-blind studies, CAB administered as a single 0.5mg dose or a total 1 mg dose, given 0.25 mg every 12 hfor 2 days, suppressed lactation in 85% of nursingmothers [7].
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
Colao, Lombardi & Annunziato 563
-3
- 2.5
-2
- 1.5
-1
- 0.5
0
Basal 18 months
Ts
co
re
BRC CV CAB
Figure 5: Bone mass evaluation shown as T score at lumbar spine in men with prolactinoma treated for 18 months with bromocriptine(BRC), cabergoline (CAB) and quinagolide (CV). Despite normal PRL and testosterone levels were achieved during treatment, nodifference in T score was noted [69].

4.3 Acromegaly
In normal subjects the administration of DA stimulatesGH secretion via a CNS-mediated mechanism [90].Conversely, at least in half of the patients withGH-secreting adenomas, DAs inhibit GH secretion,presumably through the stimulation of D2 receptors,the same as that involved in the regulation of PRLsecretion in normal and neoplastic lactotrophes[35,90]. DAs are primarily effective in thoseGH-secreting tumours that co-secrete PRL or thatexhibit immunostaining for PRL [90-93]. In a collectionof 28 series, including over 500 patients withacromegaly, bromocriptine lowered GH levels below10 µg/l in 50% of the cases, but below 5 µg/l in only 10- 20% of them [90]. It also produced a symptomaticimprovement in up to 70% of patients but tumourshrinkage occurred in only 10 - 15% of cases [35,90].Side effects, such as nausea, vomiting, posturalhypotension, nasal congestion and depressionappearing after administration of the first dose, inmost patients can be prevented by starting at lowerdoses. However, as high doses are needed fortherapeutic efficacy, side effects are often a limitingfactor. In this light, promising results have beenrecently reported with CAB treatment in acromegaly.We first reported that CAB was effective only in 1patient out of 11 treated with CAB at the dose of 2mg/week [94]. In contrast, Abs et al. [95] in amulticentre study observed that CAB at the maximalweekly dose of 3.5 mg induced the normalisation ofIGF-I levels in 39% of cases and significantly reducedIGF-I levels in another 28%. However, when theprevalence of IGF-I normalisation was evaluated inpatients with mild disease, as diagnosed on the basisof basal IGF-I concentration below 750 mg/l, it was ashigh as 53% [95] . Tumour shrinkage wasdemonstrated in 13 of 21 patients with tumourreduction of 50% in 5 GH/PRL-secreting adenomas.CAB was tolerated very well by all patients and onlytwo patients were withdrawn from treatment fornausea [95]. In another study, CAB was administeredto 18 acromegalic patients: 10 previously shown to besensitive to DA and 8 shown to be resistant to somato-statin analogues [96]. Serum GH levels weredecreased from a median value of 6.6 - 3.5 µg/l whileIGF-I values were decreased from a median value of720 - 375 µg/l [96]. Individual GH levels decreased tobelow 2 µg/l in 5 patients, and 2 - 5 µg/l in another 5patients, while IGF-I levels were suppressed below50% of baseline in 8 patients and normal age-adjustedIGF-I values were reached in 5 patients (27%) [96]. As
compared to the efficacy of bromocriptine in the 10suitable patients, a greater effectiveness of CAB wasshown as IGF-I levels decreased 46.8% on CABtreatment, and 31% on bromocriptine treatment [96].Shrinkage of GH-secreting adenoma was documentedin three patients whose pituitary imaging wasrepeated during CAB [96]. In another study usingincreasing doses of CAB, up to 3.5 mg/week, 7 out of10 patients with active acromegaly showed a fall in theGH to 33% and IGF-1 to 67% of the basal value butonly two achieved biochemical remission [97]. 4 of the10 patients were unable to tolerate the maximum doseof 1 mg daily [97].
However, as a single pharmacological approach, orwhen compared to DA, somatostatin analogues weredemonstrated to be effective in the majority ofacromegalic patients [92,98-101]. In a number ofacromegalic patients the normalisation of GH andIGF-I levels is not achieved even by using high dosesof octreotide or lanreotide. In selected acromegalicpatients, unresponsive to octreotide alone, thecombined treatment with bromocriptine orquinagolide was shown to better suppress GH/IGF-Ilevels [99,101,102], and this effect was suggested to bedue to increased bioavailability of bromocriptineduring combined administration with OCT [103].Recently, the combined treatment with lanreotide andCAB was shown to induce a significantly greaterpercent suppression of GH and IGF-I levels thanoctreotide and lanreotide treatments alone, similar tothat observed using octreotide+quinagolide but witha notably improved patients compliance [104]. In fact,normalisation of GH and IGF-I was achieved in 5 outof 10 patients with lanreotide, administered at thedose of 30 mg im. every 10 days, combined with CAB,administered at the dose of 1.5 - 3 mg/week. Asfurther support to a previous evidence [94], all thepatients who achieved the normalisation of GH andIGF-I levels after the combined lanreotide+CABtreatment showed high PRL levels or a moderate-to-intense positive PRL at immunostaining performed onsurgically removed adenomas [104]. On the otherhand, it is well known that hyperprolactinaemicacromegalics respond to dopaminergic drugs betterthan normoprolactinaemic acromegalics [105,106].
In conclusion, although the treatment with CAB inacromegaly has only been performed in a still limitednumber of patients and its efficacy is clearly reducedas compared to that displayed by somatostatinanalogues, in some selected patients, overall whenhyperprolactinaemia is present, CAB can be tested
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
564 Cabergoline

taking into consideration the low cost, as compared tosomatostatin analogues, and the easier oral route ofadministration. In peculiar cases of therapy resistance,the combined administration of depot somatostatinanalogue and CAB can be employed.
4.4 Clinically non-functioning adenomas
‘Clinically non-functioning pituitary adenomas’ (NFA)represent a very heterogeneous group of tumourssince a consistent proportion of them (up to 90%) areshown to secrete low amounts of intact FSH and LHand/or their α- and β-subunits either in vitro or in vivo[107-109]. The introduction of DAs in the medicaltherapy of NFA was based on the observation that DAreceptors are present in vitro in NFA cells, as inprolactinoma cells [110]. Bromocriptine, the first DAavailable for therapeutic purposes, was used in NFAwith disappointing results [9], likely due to the loweramount and affinity of D2 receptors expressed on NFAthan on prolactinoma cells [111]. Therefore, in NFAhigher doses and a longer treatment duration than inprolactinomas could be necessary. Only a few studieshave reported the efficacy of quinagolide in thetreatment of these tumours [112-114]. 12 patients weretreated with quinagolide, at the dose of 0.3 - 0.6mg/day: 3 patients had an NFA, 8 an α-subunitsecreting and 1 an FSH/LH-secreting adenoma.Treatment for 3 - 12 months was demonstrated toinduce reduction of gonadotropin and/or α-subunitlevels in all patients [112-114]. A significant tumourshrinkage was documented in only 4 out of 12patients. No study has been reported on the efficacyof CAB in NFA. In a preliminary experience [115], CABwas administered to 10 patients with NFA whoreceived a scintigraphy using [123I]-methoxybe-nzamide ([123I]-IBZM) prior to the therapy. [123I]-IBZMwas used to detect in vivo the presence of D2receptors on pituitary tumours [114,116-120]. A signifi-cant correlation between tracer uptake in the pituitaryadenoma and clinical response to quinagolide orbromocriptine treatment was observed in a fewselected patients with PRL-, GH- or α-subunitsecreting adenomas [114,116-120]. This approachmight be of great clinical relevance in patients withNFA, in whom the lack of biochemical markers makesthe monitoring of the efficacy of pharmacotherapyvery difficult. Among the 10 patients with NFA, nouptake was detected in 6, moderate uptake in 2 andintense uptake was observed in the remaining twopatients [115]. After 12 months of treatment withquinagolide and CAB, suppression of PRL levels was
found in all 10 patients with NFA, a significantreduction of α-subunit levels was obtained in 9 out of10 patients: in 4 out of 8 patients α-subunit levels werenormalised. A significant adenoma shrinkage wasrecorded in only 2 out of the 10 patients with NFA withintense pituitary uptake of [123I]-IBZM [115].
In conclusion, as patients affected with NFA aredifficult to monitor therapeuticallly due to the lack ofbiochemical markers of overproduction, the[123I]-IBZM scintigraphy can be proposed prior to startof treatment with quinagolide or CAB. An intense[123I]-IBZM uptake in patients affected with NFA mightbe predictive of a good response to chronic treatmentwith quinagolide or CAB [115], and the patients whomight benefit from treatment could be selected on thebasis of tracer uptake. It should be mentioned thatimmunostaining for D2 receptors has been recentlyprovided [121]. In the future, it would be investigatedwhether immunostaining for D2 receptors could behelpful to characterise the tumoural receptor status invitro on surgically removed tissues, which wouldlikely be less expensive than the in vivo methods.
4.5 Cushing’s disease and Nelson’s syndrome
Neuromodulatory agents influence ACTH secretionpredominantly by acting at the hypothalamic level.Because ACTH secretion remains under the hypotha-lamic control even in the presence of anACTH-secreting pituitary tumour, compound agonistsand antagonists on the hypothalamic-pituitary axismay still influence ACTH secretion in Cushing’sdisease [122]. Bromocriptine treatment, at dosesranging from 3.75 - 30 mg/day, was attempted inpatients with Cushing’s disease with disappointingresults. In fact, acute administration of bromocriptinein Cushing’s disease decreased plasma ACTH levels inabout half of the patients but a decrease greater than50% was reported only in 18% of patients [123]. Bettertherapeutic results have been reported using veryhigh doses of 17.5 - 40 mg/daily [124]. Bromocriptinewas also demonstrated to inhibit the proliferation ofmurine ACTH-secreting pituitary adenoma (AtT-20)cells [125]. The antitumoural activity of bromocriptinewas inhibited both by actinomycin D and cyclohexi-mide, suggesting that it was dependent on new RNAand protein synthesis. The results of DNA fragmenta-tion assays and cell cycle analysis clearlydemonstrated that bromocriptine induced apoptosisin AtT-20 cells [125]. Other dopaminergic agents havebeen shown to be more effective in comparison withbromocriptine for ACTH hypersecretion [122], but no
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
Colao, Lombardi & Annunziato 565

data are presently available for CAB. One patient withpituitary-dependent Cushing’s disease, who refusedtrans-sphenoidal surgery, was treated with CAB andketoconazole with total remission of Cushing’sdisease [126]. This patient became pregnant duringthe treatment with ketoconazole and CAB anddelivered a healthy child [126]. As in Cushing’sdisease, the medical therapy could also play a role inNelson’s syndrome could also play a role since in vitrostudies demonstrated that DAs, cyproeptadine andsodium valproate inhibited both directly or indirectlyCRH release [122,123]. A marked reduction of plasmaACTH, after a single oral dose or during a chronictreatment with bromocriptine, was observed in somepatients with Nelson’s syndrome [127-129], althoughother studies failed to demonstrate such an effect[128]. In one patient we reported that treatment withCAB for 1 year at the dose of 2 mg a day was able toinduce a complete clinical and biochemical remissionof Nelson’s syndrome [130]. CAB induced thedisappearance of the pituitary adenoma asdocumented by serial MRI (Figure 6). The withdrawalfrom CAB treatment was rapidly followed by anincrease in ACTH levels so as to induce treatmentrestart [131].
In conclusion, data on the potential use of CAB inCushing’s disease and Nelson’s syndrome are lacking.However, knowledge on the pathophysiology ofACTH secretion support a role for DA in the pharma-cotherapy of these disorders. Further data are neededto clarify this issue.
6. Tolerability
DAs are characterised by a poor tolerability profile.However, studies with CAB have reported less sideeffects than with other similar compounds. Adverseeffects were noted in up to 68% of patients withhyperprolactinaemia and 16% of puerperal women ascompared to 78 and 25%, respectively, forbromocriptine [7]. Side effects occur early, generally atthe beginning of treatment, and tend to disappearspontaneously with treatment continuation. There islarge inter-patient variation in the ability to tolerateDAs; the most sensitive being healthy subjects andwomen in the early puerperium were the least [7]. It islikely that side effects associated with DAs administra-tion are due to changes in drug concentrations in theblood [7]. In this respect CAB represents an advantageas its long half-life results in a relatively flat plasmadrug concentration [7]. The most common adverse
event in patients with hyperprolactinaemia is nauseaassociated with/without vomiting (~35%), followedby headache (~30%), and dizziness or vertigo (~25%)[7,43]. Diarrhoea, drowsiness, somnolence,paresthesia and dyspnea, are less commonly reportedand the prevalence of CAB treatment withdrawal dueto side effects is reported in less than 3% of patients[7,43]. Hypotension was reported in approximately50% of women with hyperprolactinaemia during CABor bromocriptine treatment with a median decrease ofblood pressure of 10 mmHg [53]. Generally, hypoten-sion is asymptomatic: in fact only 1 of 136 patientstreated with CAB for the inhibition of lactation [88] and3 of 254 patients treated with CAB for hyperprolac-tinaemia [53] had symptomatic hypotension. Othersevere side effects, such as thromboembolic events [7]or psychosis [132], have never been reported afterCAB treatment in patients with pituitary adenomas.Pleuropulmonary inflammatory-fibrotic syndromewas described in 3 patients [133,134]. Very recentlyconstrictive pericarditis was diagnosed in a patientwith Parkinson’s disease receiving CAB therapy at thedose of 10 mg daily [135]. After an initial misdiagnosis,the patient developed a severe pleuropulmonaryinflammatory-fibrotic syndrome, a recognised compli-cation of ergoline medications, thus suggesting acommon pathogenesis due to CAB therapy [135].
7. Regulatory affairs
CAB is presently available in the majority of countriesworldwide for the treatment of hyperprolactinaemicdisorders and inhibition of lactation. The formulationis 0.5 mg tablets taken orally.
8. Conclusions
CAB is an innovative drug for the suppression of PRLlevel and also has potential for treating GH and ACTHhypersecretion. Presently, CAB is the mostappropriate first-line treatment for macroprolac-t inomas, as had already been shown formicroprolactinomas and non-tumoural hyperprolac-tinaemia, except in poorly responsive or resistantpatients. CAB shrinks tumours and can lead to tumourdisappearance in the large majority of patients withmacroprolactinoma, so as to substantially improvevisual field defects in most patients without anyapparent damage of the residual pituitary function. Inmany cases, surgical tumour debulking is unneces-sary. In microprolactinomas, the treatment strategy
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
566 Cabergoline

should be reconsidered on the basis of the high curerate of trans-sphenoidal adenomectomy, which mightbe further improved by use of new endoscopictechniques [40,81,84,85,136]. On this basis, wecurrently propose surgery as well as pharmaco-therapy to patients with microprolactinoma (Figure7). Surgery should also be recommended for patientswho are severely intolerant to DAs. In our depart-ment, patients with macroprolactinoma are currentlytreated with CAB as first approach: surgery is consid-ered only in patients severely intolerant or resistant to
the drug, or on the basis of a precise patients’ choice(Figure 7). Whether CAB can induce a permanentcure of the disease is still unknown. It has beenreported that approximately 10% of patients remainednormoprolact inaemic even long-term afterwithdrawal from DA treatment [137] while in themajority of patients the treatment should be continuedlife-long [138]. The strong and long-lasting suppres-sion of PRL during CAB treatment allows thesuggestion that the prevalence of normoprolac-tinaemia after CAB withdrawal could be greater than
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
Colao, Lombardi & Annunziato 567
Figure 6: Serial pituitary MRI scans in a patient with Nelson’s syndrome treated with cabergoline.A: negative scan during the phase of active Cushing’s disease;B: after surgical approach to the ACTH-secreting adenoma;C: after pituitary conventional radiotherapy;D: at the diagnosis of Nelson’s syndrome made on the basis of progressively elevated ACTH levels and the appearance of a right-sidedmicroadenoma (5 x 5 x 3mm);E: after 1 year of treatment with cabergoline at the dose of 1 mg twice a week.

that previously observed with bromocriptine. Werecently observed the persistence of normoprolac-tinaemia after 1 year of CAB withdrawal in 4 out of 23patients with microprolactinoma treated with CAB for12 months [139]. On this basis, we have started atreatment protocol aiming at withdrawing CABtreatment in all patients achieving normoprolac-tinaemia and disappearance of the tumour at MRI,after at least 12 months of treatment, in order toevaluate the cure rate of CAB treatment (Figure 7).These data will be available in the near future and willbe relevant in evaluating the impact of CAB in thetreatment of hyperprolactinaemic syndromes. Incontrast, the data accumulated with CAB in thetreatment of acromegaly are still small but only those
pat ients with PRL hypersecret ion or PRLimmunostaining are likely to respond. Therefore, apreliminary characterisation of the patients who canbenefit from CAB treatment is necessary prior to startan unsuccessful trial. Similarly, CAB could beemployed in a subgroup of patients with NFA orACTH hypersecretion, but the presence of D2receptors on these tumours should be evaluatedbefore starting CAB treatment to avoid the risk ofdisappointing results. In the future, the routineapplication of immunostaining surgically removedtumour tissues for D2 expression would greatly helpin the pre-treatment characterisation of patients withacromegaly, NFA, Cushing’s disease or Nelson’ssyndrome.
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
568 Cabergoline
Microprolactinomas Macroprolactinomas
PRLnormalisation
Follow-up
high PRLlevels
PRL normalisationtumour shrinkage
Treatmentcontinuation
High PRLlevels
PRL normalisationtumor disappearance
PRL normal,no tumour
High PRL levels
Visual loss,rinoliquorrhoea,
other complications
Dose titration, controlof PRL levels monthly
for 3 months, thenquarterly. MRI follow-
up in macroHighPRL
levels
PRLnormalisation
no tumour
High PRLlevels
DA therapy
Treatmentdiscontinuation
Follow-up Treatment restart
Surgery
Surgery
Doseincrements
Follow-up
Poor toleranceresistance
Figure 7: Although the most frequently applied first-line treatment for both microprolactinomas and macroprolactinomas is based onthe use of dopamine agonists, the treatment algorithm should be differentiated considering pharmacotherapy as first choice formacroprolactinomas. Surgery could be suggested in microprolactinomas as first choice as an alternative to pharmacotherapy due to thehigh cure rate. Surgery should be employed both in micro- and macroprolactinomas proven to be resistant or intolerant to pharmaco-therapy and in patients with complications, such as sudden intratumoural haemorrhage or with cerebrospinal fluid leakage.

Acknowledgements
This study was partially supported by grant9706151106 from MURST, Rome, Italy. The authorsthank Drs G Cerbone, A Di Sarno, C Di Somma, AFaggiano, D Ferone, ML Landi, P Marzullo and RPivonello for their skilful experience in taking care ofpatients with pituitary diseases in our department.
Bibliography
Papers of special note have been highlighted as:• of interest•• of considerable interest
1. LEMBERGER L: The pharmacology of ergots: past andpresent. Fed. Proc. (1978) 37:2176-2180.
2. MANTEGANI S, BRAMBILLA E, VARASI M: Ergolinederivatives: receptor affinity and selectivity. IlFarmaco. (1999) 54:288-296.
3. BRAMBILLA E, DI SALLE E, BRIATICO G, MANTEGANI S,TEMPERILLI A: Synthesis and nidation inhibitoryactivity of a new class of ergoline derivatives. Eur. J.Med. Chem. (1989) 24:421-426.
4. DI SALLE E, ORNATI G, BRIATICO G: FCE 21336, a newergoline derivative with a potent and long-actinglowering effect on prolactin secretion in rats. J.Endocrinol. Invest. (1982) 45.
5. VANCE ML, THORNER MO: Prolactin: hyperprolacti-nemic syndromes and management. In: Textbook ofEndocrinology (2nd Edition) DeGroot LJ (Ed.), WBSaunders Co., Philadelphia, USA (1989):408-418.
6. HO KY, THORNER MO: Therapeutic applications ofbromocriptine in endocrine and neurologicaldiseases. Drugs (1988) 36:67-82.
7. RAINS CP, BRYSON HM, FITTON A: Cabergoline. Areview of its pharmacological properties andtherapeutic potential in the treatment of hyperprolac-tinaemia and inhibition of lactation. Drugs (1995)49:255-279.
8. STROLIN-BENEDETTI M, DOSTERT P, BARONE D et al.: Invivo interaction of cabergoline with rat braindopamine receptors labeled with [3H]N-n-propylnorapomorphine. Eur. J. Pharmacol. (1990)187:399-408.
9. BEVAN JS, WEBSTER J, BURKE CW et al.: Dopamineagonists and pituitary tumor shrinkage. Endocr. Rev.(1992) 13:220-240.
• A very comprehensive and accurate review on the effects ofDAs on tumour volume addressing the molecular basis fortheir shrinking effect.
10. ENJALBERT A, BOCKAERT J: Pharmacological charac-terisation of the D-2 dopamine receptor negativelycoupled with adenylated cyclase in rat anteriorpituitary. Mol. Pharmacol. (1983) 23:576-584.
11. SPADA A, NICOSIA S, CORTELLAZZI L et al.: In vitrostudies on prolactin release and adenylate cyclaseactivity in human prolactin-secreting pituitaryadenomas. Different sensitivity of macro- andmicroadenomas to dopamine and vasoactiveintestinal polypeptide. J. Clin. Endocrinol. Metab. (1983)56:1-10.
12. MCDONALD WM, SIBLEY DR, KILPATRICK BF et al.:Dopaminergic inhibition of adenylate cyclasecorrelates with high affinity agonist binding toanterior pituitary D2-dopamine receptors. Mol. Cell.Endocrinol. (1984) 36:201-209.
13. CROSIGNANI PG, FERRARI C: Dopaminergic treatmentsfor hyperprolactinemia. Baillieres Clin. Obstet. Gynaecol.(1990) 4:441-455.
14. TROUILLAS J, CHEVALLIER P, CLAUSTRAT B et al.: Inhibi-tory effects of the dopamine agonists quinagolide (CV205-502) and bromocriptine on prolactin secretionand growth of SMtTW pituitary tumors in the rat.Endocrinology (1994) 134:401-410.
15. EGUCHI K, KAWAMOTO K, UOZUMI T, ITO A, ARITA K,KURISU K: In vivo effect of cabergoline, a dopamineagonist, on estrogen-induced rat pituitary tumors.Endocr. J. (1995) 42:153-161.
16. EGUCHI K, KAWAMOTO K, UOZUMI T, ITO A, ARITA K,KURISU K: Effect of cabergoline, a dopamine agonist,on estrogen-induced rat pituitary tumors: in vitroculture studies. Endocr. J. (1995) 42:413-420.
17. JOCHLE W, ARBEITER K, POST K et al.: Effects onpseudo-pregnancy, pregnancy and interoestrousintervals of pharmacological suppression of prolactinsecretion in female dogs and cats. J. Reprod. Fertil. (1989)39(Suppl.):199-207.
18. VESTERGEN JP, ONCLIN K, SILVA LD et al.: Abortioninduction in the cat using prostaglandin F2 alpha anda new anti-prolactinic agent cabergoline. J. Reprod.Fertil. (1993) 47(Suppl.):411-417.
19. PONTIROLI AE, VIBERTI GC, MANGILI R et al.: Selectiveand extremely long inhibition of prolactin release inman by 1-ethyl-3-(3¢-dimethylaminopropyl)-3-(6¢
allylergoline-8¢-b-carbonyl)urea-diphosphate (FCE21336). Br. J. Clin. Pharmacol. (1987) 23:433-438.
20. ANDREOTTI AC, PIANEZZOLA E, PERSIANI S et al.:Pharmacokinetics, pharmacodynamics, andtolerability of cabergoline, a prolactin-lowering drug,after administration of increasing oral doses (0.5, 1.0,and 1.5 milligrams) in healthy male volunteers. J. Clin.Endocrinol. Metab. (1995) 80:841-845.
21. MELIS GB, GAMBACCIANI M, PAOLETTI AM et al.: Doserelated prolactin-inhibitory effect of the newlong-acting dopamine receptor agonist cabergoline innormal cycling, puerperal and hyperprolactinemicwomen. J. Clin. Endocrinol. Metab. (1987) 65:541-545.
22. DI SALLE E, ORNATI G, GIUDICI D et al.: Effect of the newergoline derivative FCE 21336 on prolactin and LHsecretion in the rat. J. Endocrinol. Invest. (1983) 6(Suppl.1):6.
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
Colao, Lombardi & Annunziato 569

23. FERRARI C, MATTEI A, MELIS GB et al.: Cabergoline:long-acting oral treatment of hyperprolactinemicdisorders. J. Clin. Endocrinol. Metab. (1989) 68:1201-1206.
24. FERRARI C, PARACCHI A, MATTEI AM et al.: Cabergolinein the long-term therapy of hyperprolactinemicdisorders. Acta Endocrinol. (1992) 126:489-494.
25. FALSETTI L, ZANAGNOLO V, GALBIGIANI E: Cabergolinetreatment in hyperprolactinemic women. J. Obstet.Gynecol. (1991) 11:68-71.
26. GIUSTI M, LOMEO A, TORRE R et al.: Effect of subacutecabergoline treatment on prolactin, thyroidstimulating hormone and growth hormone responseto simultaneous administration of thyrotropin-releasing hormone and growth hormone-releasinghormone in hyperprolactinemic women. Clin.Endocrinol. (1989) 30:315-321.
27. DURANTE R, GIUSTI M, CARRARO A et al.: LHRH-inducedgonadotropin release before and after short-termtherapy with cabergoline in hyperprolactinemicpatients. Minerva Endocrinol. (1991) 16:11-16.
28. DALL’ARA A, LIMA L, COCCHI D et al.: Inhibitory effect ofcabergoline on the development of oestrogen-inducedprolactin-secreting adenomas of the pituitary. Eur. J.Pharmacol. (1988) 151:97-102.
29. GIUDICI D, ZACCHEO T, ORNATI G et al.: Antitumouractivity of FCE 21336, a new prolactin lowering drug,on experimental hormone-responsive tumors. J.Steroid. Biochem. Mol. Biol. (1983) 19(Suppl.):145S.
30. FORNELLI F, ZACCHEO T, DI SALLE E et al.: Correlationbetween inhibitory effect on prolactin secretion andanti-tumour activity of new ergoline compounds onDMBA-induced tumours in rats. Eur. J. Cancer.Clin.Oncol. (1983) 19:1545-1551.
31. PERSIANI S, PIANEZZOLA E, BROUTIN F et al.: Radioim-munoassay for the synthetic ergoline derivativecabergoline in biological fluids. J. Immunoassay (1992)13:457-476.
32. PIANEZZOLA E, BELLOTTI V, LA CROIX R et al.: Determi-nation of cabergoline in plasma and urine byhigh-performance liquid chromatography withelectrochemical detection. J. Chromatogr. (1992)574:170-174.
33. COCCHIARA G, STROLIN BENEDETTI M: Excretionbalance and urinary metabolic pattern of [3H] cabergo-line in man. Drug Metab. Drug Interact. (1992) 10:199-211.
34. BATTAGLIA R, STROLIN BENEDETTI M et al.: Dispositionand urinary metabolic pattern of cabergoline, a potentdopaminergic agonist, in rat, monkey and man.Xenobiotica (1993) 23:1377-1389.
35. COLAO A, LOMBARDI G: Growth hormone andprolactin excess. Lancet (1998) 352:1455-1461.
• An up-to-date review on the most relevant clinical issues ofGH and PRL excess.
36. DELGRANGE E, MAITER D, DONCKIER J, TOURNIAIRE J:Influence of age on the clinical presentation of prolac-tinomas in male patients. Gerontology (1999) 45:160-164.
37. LEVY A, LIGHTMAN SL: Diagnosis and management ofpituitary tumors. Br. Med. J. (1994) 308:1087-1091.
38. DALKIN AC, MARSHALL JC: Medical therapy ofhyperprolactinemia. Endocrinol. Metab. Clin. North Am.(1989) 18:259-276.
39. CUNNAH D, BESSER M: Management of prolactinomas.Clin. Endocrinol. (1991) 34:231-235.
40. MOLITCH ME, THORNER MO, WILSON C: Management ofprolactinomas. J. Clin. Endocrinol. Metab. (1997)82:996-1000.
41. COLAO A, ANNUNZIATO L, LOMBARDI G: Treatment ofprolactinomas. Ann. Med. (1998) 30:452-459.
• Up-to-date reviews on the treatment strategies inhyperprolactinaemia.
42. VANCE M, EVANS W, THORNER M: Bromocriptine. Ann.Intern. Med. (1984) 100:78-91.
43. WEBSTER J: A comparative review of the tolerabilityprofiles of DA agonists in the treatment of hyperpro-lactinemia and inhibition of lactation. Drug Saf. (1996)14:228-238.
44. BRUE T, PELLEGRINI J, GUNZ G et al.: Effects ofdopamine agonist CV 205-502 in human prolac-tinomas resistant to bromocriptine. J. Clin. Endocrinol.Metab. (1992) 74:577-584.
45. VILAR L, BURKE CW et al.: Quinagolide efficacy andtolerability in hyperprolactinemic patients who areresistant to or intolerant of bromocriptine. Clin.Endocrinol. (1994) 41:821-826.
46. RASMUSSEN C, BROWNELL J, BERGHT T: Clinicalresponse and prolactin concentration in hyperprolac-tinemic women during and after treatment for 24months with the new dopamine agonist, CV 205-502.Acta Endocrinol. (1991) 125:78 -91.
47. MEROLA B, SARNACCHIARO F, COLAO A et al.: Positiveresponse to compound CV 205-502 in hyperprolacti-nemic patients resistant to or intolerant ofbromocriptine. Gynecol. Endocrinol. (1994) 8:1-7.
48. NEWMAN CB, HURLEY AM, KLEINBERG DL et al.: Effect ofCV 205-502 in hyperprolactinemic patients intolerantto bromocriptine. Clin. Endocrinol. (1989) 31:391-400.
49. CICCARELLI E, GIUSTI M, MIOLA A et al.: Effectivenessand tolerability of long-term treatment with cabergo-line, a new-lasting ergoline derivative, in hyperprolac-tinemic patients. J. Clin. Endocrinol. Metab. (1989)69:725-728.
50. MURATORI M, AROSIO M, GAMBINO G, ROMANO C,BIELLA O, FAGLIA G: Use of cabergoline in thelong-term treatment of hyperprolactinemic andacromegalic patients. J. Endocrinol. Invest. (1997)20:537-546.
51. WEBSTER J, PISCITELLI G, POLLI A et al.: The efficacy andtolerability of long-term cabergoline therapy inhyperprolactinemic disorders: an open, uncontrolled,multicentre study. Clin. Endocrinol. (1993) 39:323-329.
52. WEBSTER J, PISCITELLI G, POLLI A et al.: A comparison ofcabergoline and bromocriptine in the treatment of
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
570 Cabergoline

hyperprolactinemic amenorrhea. N. Engl. J. Med. (1994)331:904-909.
• The first paper addressing the issue of the comparisonbetween the efficacy of bromocriptine and cabergolineincluding a very large series of patients with microprolac-tinoma and non-tumoural hyperprolactinaemia.
53. VERHELST J, ABS R, MAITER D et al.: Cabergoline in thetreatment of hyperprolactinemia: a study in 455patients. J. Clin. Endocrinol. Metab. (1999) 84:2518-2522.
• The most recent paper including the largest series ofpatients with hyperprolactinaemia treated with cabergoline.
54. BILLER BMK, MOLITCH ME, VANCE ML et al.: Treatmentof prolactin-secreting macroadenomas with theonce-weekly dopamine agonist cabergoline. J. Clin.Endocrinol. Metab. (1996) 81:2338-2343.
55. FERRARI CI, ABS R, BEVAN JS et al.: Treatment ofmacroprolactinoma with cabergoline: a study of 85patients. Clin. Endocrinol. (1997) 46:409-413.
56. COLAO A, DI SARNO A, LANDI ML et al.: Long-term andlow-dose treatment with cabergoline inducesmacroprolactinoma shrinkage. J. Clin. Endocrinol.Metab. (1997) 82:3574-3579.
57. CANNAVO’ S, CURTO’ L, SQUADRITO S et al.: A firstchoice treatment in patients with previously untreatedprolactin-secreting pituitary adenoma. J. Endocrinol.Invest. (1999) 22:354 -359.
58. COLAO A, DI SARNO A, LANDI ML et al.: Macroprolac-tinoma shrinkage during cabergoline treatment isgreater in naive than in patients pre-treated with otherdopamine agonists: a prospective study in 110 patientsJ. Clin. Endocrinol. Metab. (2000). (In Press).
59. DE ROSA M, COLAO A, DI SARNO A et al.: Cabergolinetreatment rapidly improves gonadal function inhyperprolactinemic males: a comparison withbromocriptine. Eur. J. Endocrinol. (1998) 138:286-293.
60. CICCARELLI E, GROTTOLI S, RAZZORE P et al.: Long-termtreatment with cabergoline a new long-lastingergoline derivative in idiopathic or tumoroushyperprolactinemia and outcome of drug-inducedpregnancy. J. Endocrinol. Invest. (1997) 20:547-551.
61. FERRARI C, PISCITELLI G, CROSIGNANI PG: Cabergoline:a new drug for the treatment of hyperprolactinaemia.Hum. Reprod. (1995) 10:1647-1652.
62. TURKALJ I, BRAUN P, KRUPP P: Surveillance ofBromocriptine in pregnancy. JAMA (1982)247:1589-1591.
63. CORENBLUM B, DONOVAN L: The safety of physio-logical estrogen plus progestin replacement therapyand with oral contraceptive therapy in women withpathological hyperprolactinemia. Fertil. Steril. (1993)59:671-673.
64. KLIBANSKI A, NEER RM, BEITINS IZ, RIDGWAY C, ZARVASNT, MC ARTHUR JW: Decreased bone density inamenorrheic women. N. Engl. J. Med. (1980)303:1511-1514.
65. KLIBANSKI A, GREENSPAN SL: Increase in bone massafter treatment of hyperprolactinemic amenorrhea. N.Engl. J. Med. (1986) 315:542-546.
66. JACKSON JA, KLEEREKOPER M, PARFITT M: Symptomaticosteoporosis in a man with hyperprolactinemichypogonadism. Ann. Intern. Med. (1986) 105:543-545.
67. GREENSPAN SL, OPPENHEIM DS, KLIBANSKI A:Importance of gonadal steroids to bone mass in menwith hyperprolactinemic hypogonadism. Ann. Intern.Med. (1989) 110:526-531.
68. BEREZIN M, SHIMON I, HADANI M: Prolactinoma in 53men: clinical characteristics and modes of treatment.J. Endocrinol. Invest. (1995) 18:436-441.
• Prolactinomas in men are less frequent than in women andthe presentation of the clinical syndrome is partly differentas demonstrated in this paper.
69. DI SOMMA C, COLAO A, DI SARNO A et al.: Bone markersand bone density responses to dopamine agonisttherapy in hyperprolactinemic males. J. Clin.Endocrinol. Metab. (1998) 83:807-813.
70. COLAO A, DI SOMMA C, LOCHE S et al.: Prolactinomas inchildren and adolescents: persistent bone loss after 2years of prolactin normalization. Clin. Endocrinol.(2000). (In Press).
71. DELGRANGE E, CRABBE J, DONCKIER J: Late develop-ment of resistance to bromocriptine in a patient withmacroprolactinoma. Horm. Res. (1998) 49:250-253.
72. DELGRANGE E, MAITER D, DONCKIER J: Effects of thedopamine agonist cabergoline in patients with prolac-tinoma intolerant or resistant to bromocriptine. Eur. J.Endocrinol. (1996) 134:454-456.
73. COLAO A, DI SARNO A, SARNACCHIARO F et al.: Prolac-tinomas resistant to standard dopamine agonistsrespond to chronic cabergoline treatment. J. Clin.Endocrinol. Metab. (1997) 82:876 -883.
74. PELLEGRINI I, RASOLONJANAHARY R, GUNZ G et al.:Resistance to bromocriptine in prolactinomas. J. Clin.Endocrinol. Metab. (1989) 69:500-509.
75. CACCAVELLI l, FERON F, MORANGE I et al.: Decreasedexpression of the two D2 dopamine receptor isoformsin bromocriptine-resistant prolactinomas. Neuroendo-crinology (1994) 60:314-322.
76. BARLIERI A, PELLEGRINI-BOUILLER I, CACCAVELLI I et al.:Abnormal transduction mechanisms in pituitaryadenomas. Horm. Res. (1997) 47:227-234.
• A review on the abnormal transduction mechanisms inpituitary adenomas.
77. DURANTEAU L, CHANSON P, LAVOINNE A, HORLAIT S,LUBETSKI J, KUHN JM: Effects of new dopaminergicagonist CV 205-502 on plasma PRL levels and tumorsize in BRC-resistant prolactinomas. Clin. Endocrinol.(1991) 34:25-29.
78. RAZZAQ R, O’HALLORAN DJ, BEARWELL CG, SHALET SM:The effects of CV 205-502 in patients with hyperprolac-tinemia intolerant and/or resistant to bromocriptine.Horm. Res. (1993) 39:218-222.
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
Colao, Lombardi & Annunziato 571

79. CANNAVO S, BARTOLONE L, BLANDINO A, SPINELLA S,GALATIOTO S, TRIMARCHI F: Shrinkage of aPRL-secreting pituitary macroadenoma resistant tocabergoline. J. Endocrinol. Invest. (1999) 22:306-309.
80. COLAO A, LOCHE S, CAPPA M et al.: Prolactinomas inchildren and adolescents. Clinical presentation andlong term follow-up. J. Clin. Endocrinol. Metab. (1998)83:2777-2780.
81. DISSANEEVATE P, WARNE GL: Hyperprolactinaemiaand pituitary adenomas in adolescence. J. Pediatr.Endocrinol. Metab. (1998) 11:531-541.
82. MOLITCH ME: Medical treatment of prolactinomas.Endocrinol. Metab. Clin. North. Am. (1999) 28:143-169.
• Up-to-date reviews on the treatment strategies inhyperprolactinaemia.
83. JHO HD, CARRAU RL, KO Y: Endoscopic pituitarysurgery. In: Neurosurgical operative Atlas. Wilkins RH,Rengachary SS (Eds.), Park Ridge, Ill: American Associationof Neurological Surgeons (1996) 5:1-12.
84. CAPPABIANCA P, ALFIERI A, COLAO A et al.: Endoscopicendonasal transsphenoidal approach: an additionreason in support of surgery in the management ofpituitary lesions. Skull Base Surgery (1999) 9:109-117.
85. CABALLERO-GORDO A, LOPEZ-NAZARENO N,CALDERAY M et al.: Oral cabergoline-single-dose inhibi-tion of puerperal lactation. J. Reprod. Med. (1991)36:717-721.
86. MELIS GB, GAMBACCIANI M, PAOLETTI AM et al.: Doserelated prolactin-inhibitory effect of the newlong-acting dopamine receptor agonist cabergoline innormal cycling, puerperal and hyperprolactinaemicwomen. J. Clin. Endocrinol. Metab. (1987) 65:541-545.
87. GIORDA G, DEVINCENTIIS S, MOTTA T et al.: Cabergo-line versus bromocriptine in suppression of lactationafter caesarean delivery. Gynecol. Obstet. Invest. (1991)31:93-96.
88. EUROPEAN MULTICENTER STUDY GROUP FORCABERGOLINE IN INHIBITION OF LACTATION: Singledose cabergoline versus bromocriptine in inhibitionof puerperal lactation: randomized, double blind,multicenter study. Br. Med. J. (1991) 302:1367-1371.
89. MELIS GB, MAIS V, PAOLETTI AM et al.: Prevention ofpuerperal lactation by a single oral administration ofthe new prolactin-inhibiting drug cabergoline. Obstet.Gynecol. (1988) 71:311-314.
90. JAFFE CA, BARKAN AL. Acromegaly: recognition andtreatment. Drugs (1994) 47:425-445.
91. MELMED S, HO K, KLIBANSKI A, REICHLIN S, THORNERMO: Recent advances in pathogenesis, diagnosis andmanagement of acromegaly. J. Clin. Endocrinol. Metab.(1995) 80:3395-3402.
92. MELMED S, DOWLING RH, FROHMAN LA et al.:Consensus statement: benefits versus risks of medicaltherapy for acromegaly. Am. J. Med. (1994) 97:468-473.
93. WASS JAM, THORNER MO, MORRIS DV et al.: Long-termtreatment of acromegaly with bromocriptine. Br. Med.J. (1977) 1:875-878.
94. COLAO A, FERONE D, MARZULLO P et al.: Effect ofdifferent dopaminergic agents in the treatment ofacromegaly. J. Clin. Endocrinol. Metab. (1997) 82:518-523.
95. ABS R, VERSHOLST J, MAITER D et al.: Cabergoline in thetreatment of acromegaly: a study in 64 patients. J. Clin.Endocrinol. Metab. (1998) 83:374-378.
96. COZZI R, ATTANASIO R, BARAUSSE M et al.: Cabergolinein acromegaly: a renewed role for dopamine agonisttreatment? Eur. J. Endocrinol. (1998) 139:516-521.
97. JACKSON SN, FOWLER J, HOWLETT TA: Cabergolinetreatment of acromegaly: a preliminary dose findingstudy. Clin. Endocrinol. (1997) 46:745-749.
98. LAMBERTS SWJ, VAN DER LELY AJ, DE HERDER WW,HOFLAND J: Octreotide. N. Engl. J. Med. (1996)334:246-254.
99. LAMBERTS SWJ, ZWEENS M, VERSCHOOR L, DEL POZO E:A comparison among the growth hormone loweringeffect of the somatostatin analog, SMS 201-995,bromocriptine and combination of both drugs. J. Clin.Endocrinol. Metab. (1986) 63:16-19.
100. CHIODINI PG, COZZI R, DALLABONZANA D et al.:Medical treatment of acromegaly with SMS 201-995, asomatostatin analogue: a comparison withbromocriptine. J. Clin. Endocrinol. Metab. (1987)64:447-453.
101. FLØGSTAD AK, HALSE J, GRASS P et al.: A comparison ofoctreotide, bromocriptine, or a combination of bothdrugs in acromegaly. J. Clin. Endocrinol. Metab. (1994)79:461-465.
102. LOMBARDI G, COLAO A, FERONE D et al.: CV 205-502treatment in therapy-resistant acromegalic patients.Eur. J. Endocrinol. (1995) 132:559-564.
103. FREDSTORP L, KUTZ K, WERNER S: Treatment withoctreotide and bromocriptine in patients withacromegaly: an open pharmacodynamic interactionstudy. Clin. Endocrinol. (1994) 41:103-108.
104. MARZULLO P, FERONE D, MARINÒ V et al.: Effect of acombined treatment with the slow release somato-statin analog lanreotide and the selective dopamine D2
receptor agonist cabergoline in therapy resistantacromegalic patients. Pituitary (1999) 1:115-120.
105. LAMBERTS SWJ, LIUZZI A, CHIODINI PG, VERDE S, KLIJNJGM, BIRKENHÄGER JC: The value of plasma prolactinlevels in the prediction of the responsiveness ofgrowth hormone secretion to bromocriptine and TRHin acromegaly. Eur. J. Clin. Invest. (1982) 12:151-155.
106. LAMBERTS SWJ, KLIJN JGM, VAN VROONHOVEN CCJ,STEFANKO SZ, LIUZZI A: The role of prolactin in theinhibitory action of bromocriptine on growthhormone secretion in acromegaly. Acta Endocrinol.(1983) 103:446-450.
107. BECK-PECCOZ P, BRUCKER-DAVIS F, PERSANI L,SMALLRIDGE RC, WEINTRAUB BD: Thyrotropin-secreting pituitary tumours. Endocr. Rev. (1996)17:610-638.
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
572 Cabergoline

108. KWEKKEBOOM DJ, DE JONG FH, LAMBERTS SWJ:Gonadotropin release by clinically nonfunctioningand gonadotroph pituitary adenomas in vivo and invitro: relation to sex and effects of thyrotropin-releasing hormone, gonadotropin-releasinghormone, and bromocriptine. J. Clin. Endocrinol.Metab. (1989) 68:1128-1135.
109. SACCOMANNO K, GIL-DEL-ALAMO P, BASSETTI M,REZA-ELAHI F, SPADA A: In vitro detection of glycopro-tein production and secretion by human nonfunc-tioning pituitary adenomas. J. Endocrinol. Invest. (1993)16:109-115.
110. BEVAN JS, BURKE CW: Non-functioning pituitaryadenomas do not regress during bromocriptinetherapy but possess membrane-bound dopaminereceptors which bind bromocriptine. Clin. Endocrinol.(1986) 25:561- 572.
111. KOGA M, NAKAO H, ARAO M et al.: Demonstration ofspecific dopamine receptors on human pituitaryadenomas. Acta Endocrinol. (1987) 114:595-602.
112. HEDNER P, VALDEMARSSON S: Reduced size of ahormonally silent pituitary adenoma duringtreatment with CV 205-502, a new dopamine agonistmainly stimulating D2 receptors. Neurosurgery (1989)25:948-950.
113. KWEKKEBOOM DJ, LAMBERTS SWJ: Long-termtreatment with dopamine agonist CV 205-502 ofpatients with clinically non-functioning, gonado-troph, or a-subunit secreting pituitary adenoma. Clin.Endocrinol. (1992) 36:171-176.
114. FERONE D, LASTORIA S, COLAO A et al.: Correlation ofscintigraphic results using 123I-methoxybenzamidewith hormone levels and tumor size response toquinagolide in patients with pituitary adenomas. J.Clin. Endocrinol. Metab. (1998) 83:248-252.
115. COLAO A, FERONE D, LASTORIA S et al.: Hormone levelsand tumor size response to quinagolide and cabergo-line in patients with prolactin-secreting and clinicallynonfunctioning pituitary adenomas: predictive valueof pituitary scintigraphy with 123I-Methoxy-benzamide. Clin Endocrinol (2000). (In Press).
116. SCILLITANI A, DICEMBRINO F, DI FAZIO P et al.: In vivovisualization of pituitary dopaminergic receptors byiodine-123 methoxybenzamide (IBZM) correlates withsensitivity to dopamine agonists in two patients withmacroprolactinomas. J. Clin. Endocrinol. Metab. (1995)80:2523-2525.
117. DE HERDER WW, REIJST AEM, KWEKKEBOOM DJ et al.: Invivo imaging of pituitary tumours using a radiola-belled dopamine D2 receptor radioligand. Clin.Endocrinol. (1996) 45:755-767.
118. DE HERDER WW, REIJST, AEM, DE SWART J et al.:Comparison of iodine-123 epidepride and iodine-123IBZM for dopamine D2 receptors imaging inclinically non-functioning pituitary macroadenomasand macroprolactinomas. Eur. J. Nucl. Med. (1999)26:46-50.
119. VERHOEFF NP, BEMELMAN FJ, WIERSINGA WM, VANROYEN EA: Imaging of dopamine D2 and somatostatinreceptors in vivo using single-photon emissiontomography in a patient with TSH/PRL-producingpituitary macroadenoma. Eur. J. Nucl. Med. (1993)20:555-561.
120. PIRKER W, RIEDL M, LUGER A et al.: Dopamine D2
receptor imaging in pituitary adenomas using Iodine-123-Epidepride and SPECT. J. Nucl. Med. (1996)37:1931-1937.
121. KHAN ZU, GUTIERREZ A, MARTIN R, PENAFIEL A, RIVERAA, DE LA CALLE A: Differential regional and cellulardistribution of dopamine D2-like receptors: animmunocytochemical study of subtype-specificantibodies in rat and human brain. J. Comp. Neurol.(1998) 21:353-371.
122. SONINO N, BOSCARO M: Medical therapy for Cushing’sdisease. In: Advances in Pituitary Tumour Therapy. MolitchME (Ed.), (1999):211-222.
123. KRIEGER DT: Physiopathology of Cushing’s disease.Endocr. Rev. (1983) 4:22-43.
124. MERCADO-ASIS LB, YASUDA K, MURAYAMA M et al.:Beneficial effects of high daily dose bromocriptine inCushing’s disease. Endocrinol. Jpn. (1992) 39:385-395.
125. YIN D, KONDO S, TAKEUCHI J, MORIMURA T: Inductionof apoptosis in murine ACTH-secreting pituitaryadenoma cells by bromocriptine. FEBS Lett. (1994)339:73-75.
126. BERWAERTS J, VERHELST J, MAHLER C, ABS R: Cushing’ssyndrome in pregnancy treated by ketoconazole: casereport and review of the literature. Gynecol. Endocrinol.(1999)13:175-182.
127. DORNHORST A, JENKINS JS, LAMBERTS SWJ et al.: Theevaluation of sodium valproate in the treatment ofNelson’s syndrome. J. Clin. Endocrinol. Metab. (1983)56:985-991.
128. LAMBERTS SWJ, BIRKENHAGER JC: Bromocriptine inNelson’s syndrome and Cushing’s disease. Lancet(1976) 2:811.
129. LAMBERTS SWJ, KLIJN JGM, DE QUIJADA M et al.: Themechanism of the suppressive action ofbromocriptine on adrenocorticotropin secretion inpatients with Cushing’s disease and Nelson’ssyndrome. J. Clin. Endocrinol. Metab. (1980) 51:307-311.
130. WHITEHEAD HM, BEACOM R, SHERIDAN B, ATKINSONAB: The effect of cyproheptadine and/orbromocriptine on plasma ACTH levels in patientscured of Cushing’s disease by bilateral adrenalectomy.Clin. Endocrinol. (1990) 32:193-201.
131. PIVONELLO R, FAGGIANO A, DI SALLE F, FILIPPELLA M,LOMBARDI G, COLAO A: Complete remission ofNelsons’ syndrome after 1 year treatment withcabergoline: a case report. J. Endocrinol. Invest. (1999)22:860-865.
132. TURNER TH, COOKSON JC, WASS JAH, DRURY PL, PRICEPA, BESSER GM: Psychotic reactions during treatment
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
Colao, Lombardi & Annunziato 573

of pituitary tumours with dopamine agonist. Br. Med. J.(1984) 289:1101-1103.
133. BHATT MH, KEENAN SP, FLEETHAM JA et al.: Pleuropul-monary disease associated with dopamine agonisttherapy. Ann. Neurol. (1991) 30:613-616.
134. FRANS E, DOM R, DEMEDTS M: Pleuropulmonarychanges during treatment of Parkinson’s disease witha long-acting ergot derivative, cabergoline. Eur. Respir.J. (1992) 5:263-265.
135. LING LH, AHLSKOG JE, MUNGER TM, LIMPER AH, OH JK:Constrictive pericarditis and pleuropulmonarydisease linked to ergot dopamine agonist therapy(cabergoline) for Parkinson’s disease. Mayo Clin. Proc.(1999) 74:371-375.
136. LIUZZI A, OPPIZZI G: Microprolactinomas: whyrequiem for surgery? J. Endocrinol. Invest. (1996)19:196-198.
• The indications for surgery in microprolactinomas are likelyunderestimated as underlined in this brief paper.
137. VAN’T VERLAAT JW, CHROUGHS RJ: Withdrawal ofbromocriptine after long-term therapy for macropro-lactinomas; effect on plasma prolactin and tumoursize. Clin. Endocrinol. (1991) 34:175-178.
138. FAGLIA G: Should dopamine agonists treatment forprolactinomas be life-long? Clin. Endocrinol. (1991)34:173-174.
139. DI SARNO A, LANDI ML, MARZULLO P et al.: The effect ofquinagolide and cabergoline, two selective dopaminereceptor type-2 agonists, in the treatment of prolac-tinomas. Clin. Endocrinol. (2000). (In Press).
Annamaria Colao† , Gaetano Lombardi & Lucio Annunziato† Author for correspondenceDepartment of Molecular and Clinical Endocrinology andOncology, ‘Federico II’ University, via S Pansini 5, 80131 Napoli,ItalyTel.: +39 81 7462132; Fax: +39 81 7463668;E-mail: [email protected]
© Ashley Publications Ltd. All rights reserved. Exp. Opin. Pharmacother.(2000)1(3)
574 Cabergoline